This basic idea after this surgery is to remove all visible endometriotic lesions in the pelvis and abdomen. This concept is similar to the cancer surgery where all the visible cancerous lesions are removed. The extent of surgery depends on the how far the disease has spread and what is the extent/depth of involvement of surrounding organs.
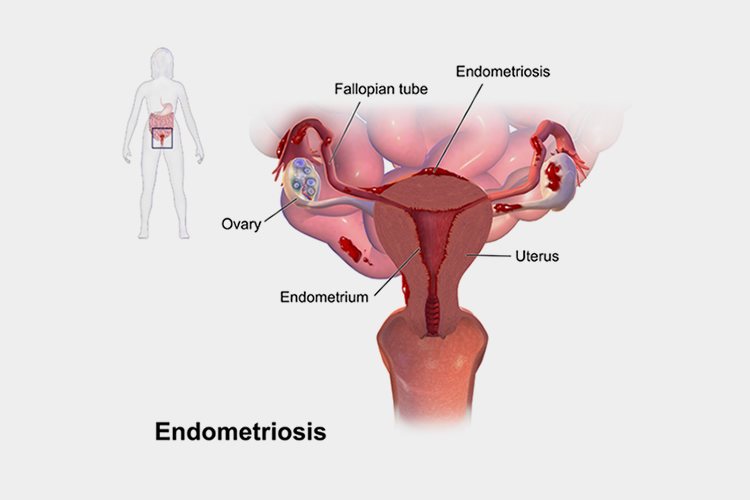
Deep infiltrating endometriosis (DIE) is a subperitoneal invasion of endometrial glands and stroma. Resulting endometriotic nodules may develop on the uterosacral ligaments, rectovaginal septum, retrocervical areas, parametrium, ureters, bowels (most commonly rectum and sigmoid colon) and less commonly in the urinary bladder, thoracic, and neural regions(sacral/obturator nerve). Genetics, age of woman, patient factors, multiple treatments with fertility drugs(ovulation induction), multiple surgeries involving uterus, and environmental factors decide the progression of the disease. DIE manifests with numerous symptoms, which are similar to unrelated diseases, such as dysmenorrhea, dyspareunia, repeated urinary tract infections around the time of periods, and subfertility. Transvaginal ultrasound, and MRI may detect and differentiate endometriosis lesions from other diseases with similar presentation. Treatment typically involves excision by laparoscopic surgery and hormonal therapy in few selected patients. These are aimed to improve the quality of life and to address individual fertility plans.
Nodule is a long-term sequel of endometriosis. It usually contains endometrial gland and fibrotic tissue which makes it resistant to medical treatment. Due to retrograde menstrual flow, the menstrual blood is deposited in pelvic cavity to most dependable areas (uterosacral ligaments, rectovaginal septum, anterior wall of rectum, parametrium, pouch of Douglas and surrounding vital organs). Due to altered genetic signals and autocrine effect of endometrial glands, these tissue starts growing and produces inflammation and release inflammatory cytokines. Theses cytokines are the reason for pelvic pain and pelvic discomfort in women with endometriosis. This inflammation heals with fibrosis which will produce dense adhesions between the organs and different structures. Endometrial glands surrounded by irregular fibrosis which is resistant to hormonal treatment is called nodule.
No. As defined by healthcare government, a specialist is a practitioner who “focuses on a specific area of medicine or a group of patients to diagnose, manage, prevent or treat certain types of symptoms and conditions.” The emphasis, however, should be on those who can actually demonstrate high volume, significant levels of knowledge, skill and dedicated care for the endometriosis disease; it is in that setting the term ‘Endometriosis specialist’ is used.
No, it is not new. It is the well-established surgical component of a multidisciplinary approach to treat endometriosis. Dedicated endometriosis surgeons have been using the excisional approach for almost 20 years now. The principles of Laparoscopic surgery itself was even reported more than 100 years ago. Jumping to the early 1930’s, the first reports of Laparoscopic interventions for non-diagnostic purposes were published. Even in 1850s, physicians were observed to ‘excise the endometriosis nodules with scissors or even with their own fingernails’.
The word cure is not used in relation to endometriosis treatment. However, excision/surgery is the gold standard treatment specifically for Deep Endometriotic lesions and is highly effective in providing relief in terms of pain, menstrual irregularities, subfertility, chronic fatigue and weakness due to endometriosis.
All surgeons – and surgeries – are not same. Remarkable confusion often arises around the surgical approaches for endometriosis. The laser is a TOOL used in performing the surgery – not a METHOD. Laparoscopy is a surgical approach, not a tool. It is important to understand that tool and method are not as important as skill of the surgeon: if surgeon can’t excise, they can’t excise using any method or tool. Be sure you know which approach they are using. The CO2 laser can be used safely and successfully perform Laparoscopic excision of all endometriosis or it can be used to ablate the surface lesions. The laser can be used in patients with borderline AMH (limited ovarian reserve) with endometrioma in the option of excision of endometrioma.
In most of instances Laser ablation and other superficial methods commonly performed by non-specialists char the surface tissue, and leaving behind endometriosis – leading to high recurrence and potential complications in future surgical interventions. Excision is routinely not often performed outside the tertiary specialty centers, so it is important to know which method your surgeon is using and understand his disease knowledge, approach and expected outcomes.
One has to understand the bias prevalent surrounding the endometriosis. Often ‘killer menstrual cramps’ are ‘normal’, or ‘in your head’. Obviously, this will cause major negative impact on quality of life, especially in the aspects of pain and psychosocial well-being.
In the general healthcare professionals including at the OB/GYN level, it is taught and hence practiced that the most common treatment are tablets suppressing the disease and performing the incomplete surgery. The disease does not simply ‘disappear” as a result of drug suppression. At best, such tablets provide only a temporary solution for symptom improvement, not the definitive treatment.
Poor outcomes for excision surgery after suppression therapies are routine and medicines that can destroy endometriosis permanently has yet to be searched. Hormonal suppression has “no effect on adhesion and infertility. Despite the evidence, some providers prefer medical management and adopt a strategy of ‘treat without seeing’ through hormone suppression.
In the majority of such cases, diagnosis, definitive treatment is delayed and patient dissatisfaction is highly common. Such medications can suppress the disease on a short-term basis, and symptoms undoubtedly reappear at cessation of tablets.
Poor surgical outcome is also another concern where incomplete or poorly performed surgery follow which the patient has to deal with any residual symptoms of the endometriosis left behind. Removing only Superficial disease is not excisional and allows for subsequent adhesion formation to bury remaining disease. Such new adhesions and new inflammation due to superficial ablation performed by inexperienced specialist increase the pain, leaving a dissatisfied patient. Burning/ablation, coagulation and other superficial treatments– with or without medical suppression -can result into poor outcomes. Surgery when appropriate, performed by the proper hands, and for the right patient can provide the best outcome for the patient.
Endometriosis surgery needs a balance between complete excision and prevention of complications during and after surgery with preservation of bladder and bowel functions and fertility. This critical decision needs surgical judgement which is based on surgical anatomy knowledge, in depth knowledge about pathogenesis of endometriosis disease and varies with the skills and experience of the gynec laparoscopic surgeon.